What is Hernia and How Can It Be Treated with Laparoscopy?
December 3, 2025 What is Hernia and How Can It Be Treated with Laparoscopy? Executive Summary: The Structural Integrity of the…

November 19, 2025

For many individuals struggling with severe obesity, the journey can feel like a lonely and frustrating battle. You may have been told that the solution is simply to “eat less and move more.” However, medical science tells a different story.
For people with class III obesity, achieving and sustaining significant weight loss through diet and exercise alone is “nearly impossible”. This is not a failure of willpower, but a matter of biology. Once the body registers a higher weight as “normal,” it actively fights to return to that weight, creating a difficult biological set point.
If this sounds familiar, it is important to know that you are not alone and that there is a powerful, effective, and life-changing solution.
Bariatric surgery, also known as weight loss surgery, is recognized as the most successful and durable long-term treatment for severe obesity. It is not a “quick fix” or a cosmetic procedure; it is a “life-saving procedure” that treats the underlying biology of obesity. However, it is a tool, not a magic wand. Its success depends on a lifelong partnership between you, your surgeon, and your commitment to a new, healthier lifestyle.
This comprehensive guide is designed to give you an honest, medically-backed understanding of this transformative journey. This information is presented from the perspective of Dr. Ramesh Makam’s practice, a pioneer with over 35 years of experience who introduced Gastric Bypass Surgery to India and holds a world record in Banded Sleeve Gastrectomies. As a leading bariatric surgeon in Bangalore, Dr. Makam is dedicated to providing a compassionate, patient-focused, and holistic approach to metabolic wellness.
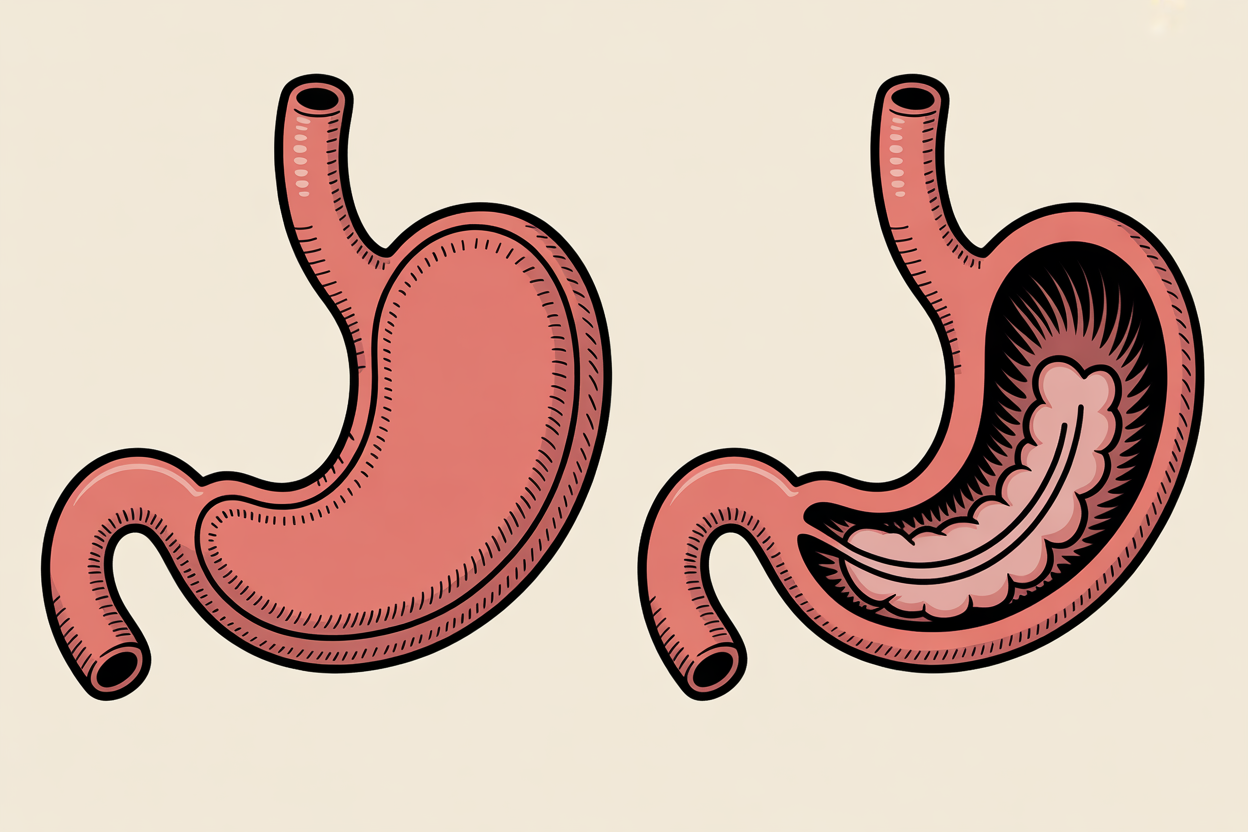
At its simplest, bariatric surgery is a group of operations that help you lose weight by making changes to your digestive system, specifically your stomach and sometimes your small intestine.
However, in modern medicine, the term is now used interchangeably with “metabolic surgery”. This is a critical distinction. The true goal of these procedures is not just to reduce the number on a scale, but to treat and prevent the cluster of “metabolic diseases related to obesity”. Dr. Makam’s practice is founded on this “Bariatric and Metabolic” philosophy, focusing on your complete health transformation.
Bariatric surgery is effective because it works in three powerful ways to reset your body’s biology:
This hormonal reset is why, after surgery, many patients find they “lose many of their improper food cravings” and “rarely do people feel deprived”. Your body is no longer fighting you; it is finally working with you.
The primary reason to consider this obesity treatment is the dramatic and life-saving improvement in your overall health. The goal is not just to lose weight, but to gain health. Dr. Makam’s holistic approach is focused on this “overall health enhancement”.
The metabolic impact of bariatric surgery is its greatest benefit:
The health benefits extend to nearly every system in the body:
The combined result of these benefits is a “marked improvement in quality of life”. Patients report boosted self-esteem, improved mental health, and more energy. Most importantly, studies show that bariatric surgery can increase your life expectancy, reducing the risk of premature death by 30-50%.
Determining if you are a candidate for bariatric surgery involves a comprehensive medical evaluation. While general guidelines exist, the criteria in India are specific.
In 2022, the leading international bariatric societies (ASMBS and IFSO) updated their 30-year-old guidelines, making them more inclusive. The current recommendations state that surgery should be an option for:
This is the most critical information for patients in India. Medical experts have recognized that Asian and Indian populations have a different body composition (more visceral fat) and “need a more aggressive approach” to treatment. In this population, serious metabolic diseases like diabetes begin at a “relatively lower BMI”.
For example, in India, a “healthy” BMI is considered 18.5-22.9, and “obesity” begins at a BMI of 25.
Because of this, the Obesity and Metabolic Surgery Society of India (OSSI) and other Asian consensus groups have established different guidelines:
This last point is crucial. A patient in Bangalore with a BMI of 28 and uncontrolled diabetes may be a prime candidate for life-saving metabolic surgery, even though most international websites would tell them they do not qualify.
Table 1: Bariatric Surgery Eligibility (General vs. Indian Guidelines)
Patient Profile | General (US/EU) Guideline (BMI) | Indian (OSSI) Guideline (BMI) |
Obesity with No Comorbidities | 35 or higher | 37.5 or higher |
Obesity with Comorbidities (e.g., T2D) | 30 or higher | 32.5 or higher |
Uncontrolled T2D with Lower BMI | Not typically covered | 27.5 or higher may be considered |
A BMI number only opens the door. A truly good candidate for surgery is someone who:
Surgery may be contraindicated for individuals with certain unmanaged psychiatric conditions, active drug or alcohol dependency, or those who are not able to commit to the required follow-up.
There are several types of bariatric surgery. The choice is a complex medical decision based on your unique health profile (e.g., your weight, your existing conditions like diabetes or acid reflux, and your goals). This is where consultation with an experienced surgeon is vital. Dr. Makam’s practice in Bangalore offers unparalleled expertise across a range of procedures, ensuring you receive the operation that is right for you.
For specific patient needs, other options exist:
Patients often ask about the Adjustable Gastric Band (Lap-Band), where a silicone band is placed around the top of the stomach. It is important to know that this procedure has “largely fallen out of favor”.61 It produced only “modest weight loss” and had very high rates of long-term complications, failures, and re-operations.
A critical clarification: This obsolete “Lap-Band” is not the same as the “Banded Sleeve Gastrectomy,” an advanced procedure for which Dr. Ramesh Makam holds a world record. Dr. Makam’s expertise is in a specialized, modern technique, not the outdated Lap-Band.
Table 2: Comparison of Common Bariatric Procedures
Procedure | How it Works (Mechanism) | Avg. Excess Weight Loss | Key Pros | Key Cons |
Sleeve Gastrectomy (LSG) | Restrictive & Hormonal | 60-70% | Simpler; No rerouting; Lowers hunger hormone. | Irreversible; Can worsen acid reflux (GERD). |
Gastric Bypass (RYGB) | Restrictive & Malabsorptive | 50-80% | Best for T2D remission; Cures GERD. | More complex; Higher risk of nutrient deficiency; Risk of dumping syndrome. |
BPD/DS | Restrictive & Highly Malabsorptive | 70-80%+ | Highest weight loss; Best for T2D remission. | Highest risk of severe, lifelong nutritional deficiencies; Complex surgery. |

A comprehensive obesity treatment plan considers all pathways. Surgery is not the only solution, but it is the most effective for severe obesity. Here are the other options.
This is the foundation of all weight loss, and a requirement both before and after surgery. A professional, medically supervised program involves customized diet plans, nutrition counseling, and exercise guidance tailored to your health.
These are minimally invasive, outpatient procedures performed with an endoscope (a flexible tube through your mouth) with no external incisions.68 They are excellent options for patients with a lower BMI (30-40) who may not qualify for surgery or who do not want a surgical procedure.
You have likely heard about the new, “highly effective” injectable medications like Semaglutide (Wegovy) and Tirzepatide (Zepbound). These GLP-1 drugs are a fantastic medical advancement, providing 15-22% weight reduction in trials.
However, it is crucial to understand two things:
While these drugs are a great tool, “metabolic and bariatric surgery remains the most effective and durable treatment for severe obesity”.
The surgery is Day 1. The rest of your life is the true journey. Success is built on an understanding that obesity is a chronic disease that requires lifelong management. The surgery is the tool that makes this management possible.
Thanks to minimally invasive laparoscopic techniques, recovery is much faster than patients expect.
Table 3: The 4 Stages of Your Post-Bariatric Diet
Stage | Timeframe | What You Eat | Key Goal |
1: Clear Liquids | Hospital / First few days | Water, clear broth, sugar-free drinks | Hydration |
2: Full Liquids | Weeks 1-2 | Protein shakes, milk, yogurt, thin soups | Hydration + Start Protein |
3: Pureed Foods | Weeks 2-4 | Scrambled eggs, mashed vegetables, pureed | |
meats | Healing & Toleration |
| 4: Soft Foods | Weeks 4-8 | Ground meat, flaked fish, soft fruits, cooked
veg 81 | Transition to Solid Food |
This is the most critical component of long-term health and is non-negotiable for life.
The decision to have bariatric surgery is one of the most important decisions you will ever make for your health. The skill, experience, and philosophy of your surgeon are paramount.
Dr. Ramesh Makam is not just a surgeon; he is a true pioneer in laparoscopic and bariatric surgery in India. When you choose his practice, you are choosing a leader with:
Your journey to health is the most important one you can take. Begin that journey with a consultation with a true pioneer and one of India’s most trusted experts.
Contact Dr. Ramesh Makam’s office at Arka Anugraha Hospital in Bangalore today to schedule your comprehensive evaluation and take the first step toward reclaiming your health.
Q: How much does bariatric surgery cost in Bangalore?
A: The cost of bariatric surgery in Bangalore can vary significantly based on the specific procedure (e.g., Sleeve vs. Bypass), the hospital, and other factors. On average, the cost can range from approximately INR 2,00,000 to INR 4,50,000.104 A precise, personalized quote can only be provided after a full consultation and evaluation.
Q: Is bariatric surgery covered by health insurance in India?
A: Yes. Following the 2019 IRDAI guidelines, most health insurance policies in India are now mandated to cover bariatric surgery, provided it is medically necessary and not for cosmetic purposes. Generally, you are eligible for coverage if your BMI is 40 or higher, or if your BMI is 35 or higher and you have at least one significant comorbidity like Type 2 Diabetes, hypertension, or sleep apnea. A policy waiting period may apply.
Q: What is “dumping syndrome”?
A: Dumping syndrome is a side effect most common after Gastric Bypass surgery. It is a group of symptoms like nausea, cramping, dizziness, and a rapid heart rate that happens when food especially sugar “dumps” from the stomach pouch into the small intestine too quickly. It is not dangerous and is effectively managed by avoiding high-sugar and high-fat foods.
Q: Can I get pregnant after bariatric surgery?
A: Yes. In fact, fertility often improves dramatically after weight loss surgery. However, it is strongly recommended that you wait 12 to 24 months after your surgery before trying to conceive. This allows your weight to stabilize and ensures your body has the nutritional stores needed for a healthy pregnancy.
Q: Will I lose my hair after weight loss surgery?
A: It is common to experience some temporary hair thinning (a condition called telogen effluvium) about 3-6 months after surgery. This is not permanent hair loss. It is a temporary response by the body to the stress of surgery and rapid weight loss. The hair will grow back as your weight and nutrition stabilize, especially if you are diligent with your protein and vitamin intake.
Q: How long is the recovery from bariatric surgery?
A: With modern minimally invasive (laparoscopic) techniques, recovery is relatively fast. Most patients stay in the hospital for 1-2 nights. You will be encouraged to walk the same day as your surgery. Most patients can return to a desk job or light activity within 2-4 weeks, though you will have restrictions on heavy lifting for longer.
BEST Institute was started with the intention of sharing my knowledge with
other fellow surgeons. During this journey, many conferences and workshops
have been conducted. Skills training is the highlight of this Institute.
December 3, 2025 What is Hernia and How Can It Be Treated with Laparoscopy? Executive Summary: The Structural Integrity of the…
November 19, 2025 What is Bariatric Surgery and Who Should Consider It? What is Bariatric Surgery and Who Should Consider It?…
October 2, 2024 NATIONAL CONFERENCE & WORKSHOP ON HERNIA Blog Dates: 27th& 28th March 1999 Venue: St. Martha’s Hospital, Bangalore This…