What is Hernia and How Can It Be Treated with Laparoscopy?
December 3, 2025 What is Hernia and How Can It Be Treated with Laparoscopy? Executive Summary: The Structural Integrity of the…

December 3, 2025
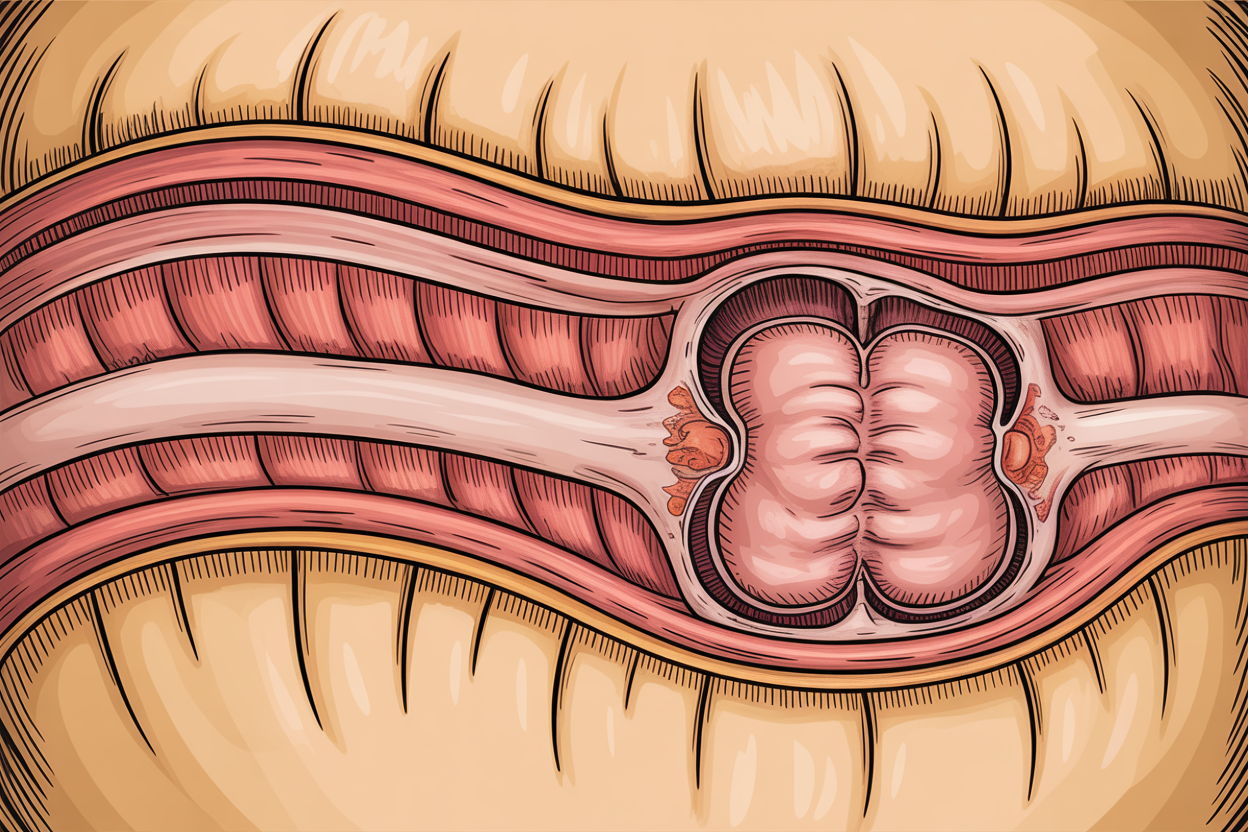
The human abdominal wall is a marvel of biological engineering, designed to contain high-pressure visceral organs while allowing for the complex range of motion required for daily life. However, this dynamic containment system is susceptible to structural failure. A hernia, often dismissed in colloquial terms as a simple “rupture” or “bulge,” represents a profound breach in this anatomical integrity. It is a condition where the internal contents of the abdomen—typically intestine or omental fat—protrude through a congenital or acquired defect in the fascia, the strong connective tissue layer that acts as the body’s internal girdle.1
For patients in Karnataka, and specifically those traversing the medical corridor between Mysore and Bangalore, the diagnosis of a hernia often brings a cascade of questions regarding urgency, surgical methodology, and long-term outcomes. The evolution of hernia surgery from a procedure fraught with recurrence and pain to a sophisticated, minimally invasive art form is one of the great success stories of modern medicine.
This report serves as a definitive, encyclopedic resource for patients and medical peers alike. Authored from the perspective of the clinical experts at ARKA Anugraha Hospital, recognized as South India’s only Center of Excellence by the Asia Pacific Hernia Society (APHS) 3, this document goes beyond the surface level. We will explore the cellular mechanisms of collagen failure that predispose individuals to herniation, the physics of laparoscopic mesh placement, the economic nuances of healthcare in Bangalore versus Mysore, and the integration of functional medicine into surgical recovery. Under the leadership of Dr. Ramesh Makam, a surgeon with over 35 years of experience and thousands of successful repairs, ARKA Anugraha stands at the forefront of this surgical evolution.
To understand the solution, one must first deeply comprehend the problem. A hernia is not merely a hole; it is a failure of the complex laminate structure of the abdominal wall.
The abdominal wall is constructed of multiple layers, each providing specific structural resistance:
The abdomen functions as a pressurized hydraulic cylinder. Intra-Abdominal Pressure (IAP) fluctuates constantly. Resting pressure is low (5-7 mmHg), but activities like coughing, sneezing, lifting weights, or straining during defecation can spike IAP to over 100-150 mmHg.
Modern research indicates that herniation is often a systemic disease of the connective tissue, not just a local mechanical failure.
The term “hernia” is an umbrella classification for various defects, each with unique anatomical characteristics and risks. At ARKA Anugraha, distinguishing the specific subtype is the first step in tailoring the laparoscopic approach.
Inguinal hernias are the most prevalent, accounting for 75% of all abdominal wall hernias. They occur in the inguinal canal, a passage in the anterior abdominal wall that conveys the spermatic cord in men and the round ligament in women.
Type | Pathophysiology | Anatomical Landmark | Risk Profile |
Indirect Inguinal | Congenital patent processus vaginalis. The sac travels through the deep inguinal ring along the spermatic cord. | Lateral to the Inferior Epigastric Vessels. | High risk of strangulation due to the tight internal ring. Common in children and young adults. |
Direct Inguinal | Acquired weakness of the posterior floor of the inguinal canal (Transversalis fascia). | Medial to the Inferior Epigastric Vessels (Hesselbach’s Triangle). | Lower risk of strangulation as the defect is often broad. Common in older men due to tissue aging. |
Pantaloon | A combined Direct and Indirect hernia occurring simultaneously on the same side. | Straddles the Inferior Epigastric Vessels. | Requires extensive repair covering both defects; ideal for laparoscopic TEP/TAPP. |
Femoral hernias occur just below the inguinal ligament, entering the femoral canal medial to the femoral vein.
Accurate diagnosis is the cornerstone of effective treatment. While a large bulge may be obvious, understanding the contents and the anatomy of the defect prevents surgical surprises.
The journey begins with a physical examination at our JP Nagar facility.
At ARKA Anugraha, we utilize advanced imaging when the clinical picture is equivocal or for surgical planning in complex cases.
The history of hernia surgery is a history of humanity’s struggle against biomechanics.
For a century, surgeons used the Bassini or Shouldice techniques. These involved suturing the edges of the muscle defect together.
The introduction of synthetic mesh (Lichtenstein repair) changed everything. Instead of pulling the edges together, a mesh was placed over the hole like a patch. This was “tension-free.” The mesh acts as a scaffold for the body’s own fibroblast cells to grow into, creating a new, reinforced layer of fascia.
While the Lichtenstein repair was effective, it still required a significant incision (5-10 cm), cutting through skin and superficial nerves. Laparoscopic repair took the concept of tension-free mesh repair and moved the access point to the inside.
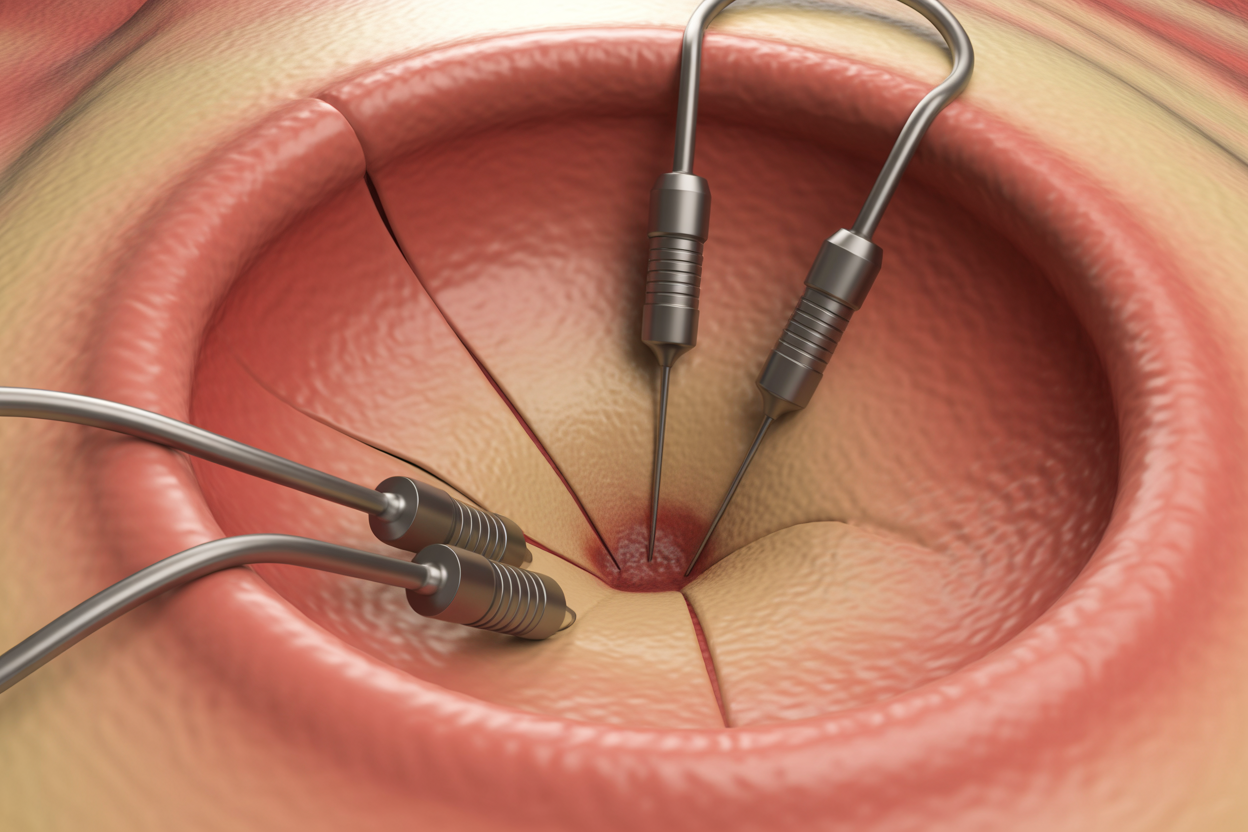
At ARKA Anugraha Hospital, laparoscopic repair is the default standard of care for inguinal and many ventral hernias. Dr. Ramesh Makam and his team are proficient in the two primary laparoscopic approaches, choosing the optimal one based on patient anatomy.
For umbilical and incisional hernias, the IPOM (Intraperitoneal Onlay Mesh) technique is used.
Not all meshes are created equal. As a Center of Excellence, ARKA Anugraha utilizes a spectrum of implant technologies tailored to the specific needs of the patient.
How the mesh is held in place is critical for preventing pain.

In the crowded healthcare market of Bangalore, ARKA Anugraha Hospital distinguishes itself through accreditation, expertise, and a unique philosophy of care.
Being recognized by the Asia Pacific Hernia Society (APHS) is a rigorous process. It verifies that:

Surgery is a trauma, albeit a controlled one. At ARKA Anugraha, we believe that a successful surgery is only half the battle; the other half is the host’s response. This is where Dr. Gaurang Ramesh’s Functional Medicine approach becomes a game-changer.
Before the first incision is made, we optimize the patient’s biology:
Post-surgery, patients have access to therapies that reduce inflammation and stress without relying solely on opioids or painkillers:
This “whole-person” approach is what sets ARKA apart from centers that view the patient merely as a “hernia case.”
A significant portion of our patient base travels from Mysore, Mandya, Coorg, and other parts of Karnataka. We recognize the logistical anxiety this entails and have streamlined the process to be as smooth as the surgery itself.
While Mysore has excellent medical facilities like Apollo BGS and Manipal Hospital 11, the super-specialized nature of complex hernia repair—especially for recurrent hernias or those requiring advanced component separation—often necessitates a referral to a dedicated Center of Excellence. The distance is negligible (approx. 145 km), but the difference in long-term outcomes for complex cases can be substantial.
We understand that cost is a decisive factor. Transparency in billing is a core value at ARKA Anugraha.
The cost of laparoscopic hernia repair varies based on complexity, the type of mesh selected, and the room category.
Procedure Type | Standard Package (₹) | Premium Package (₹) | Key Cost Drivers |
Open Inguinal Repair | ₹70,000 – ₹85,000 | ₹90,000+ | Anesthesia type, hospital stay duration (longer for open). |
Laparoscopic Inguinal | ₹90,000 – ₹1,20,000 | ₹1,50,000+ | Mesh Type (Standard vs. 3D Anatomical), Fixation device (Tacks/Glue). |
Laparoscopic Umbilical | ₹80,000 – ₹1,00,000 | ₹1,20,000+ | Composite Mesh cost (significantly higher for ventral hernias). |
Complex Incisional | ₹1,50,000 – ₹2,50,000 | ₹3,00,000+ | Component separation, extended OR time, ICU stay if needed. |
Data synthesized from market analysis snippets.
Note: These are estimates; final billing depends on individual case specifics.
Patients sometimes ask, “Why is laparoscopy more expensive?”
Recovery is a partnership between the surgeon and the patient. While the surgery fixes the defect, your adherence to post-op protocols ensures the repair lasts a lifetime.
Constipation is the enemy of hernia repair. Straining puts immense pressure on the fresh mesh.
Meal | Suggestions |
Breakfast | Oatmeal / Daliya / Idli (fermented foods are good for gut) with weak sambar. |
Mid-Morning | Papaya (excellent natural laxative) or Tender Coconut Water. |
Lunch | Khichdi (easy to digest), Moong Dal soup, small portion of steamed vegetables (gourd/lauki). |
Snack | Roasted Makhana or clear soup. Avoid fried snacks. |
Dinner | Light soup, steamed fish or scrambled egg whites. Keep dinner light. |
Answer: “Watchful waiting” is an option for asymptomatic inguinal hernias in men, but it carries risks. Hernias never heal on their own; they only get bigger. Surgery becomes more complex as the defect widens. Furthermore, there is a small but unpredictable risk of strangulation. Elective repair is always safer and has better outcomes than emergency surgery.
Answer: Laparoscopy involves inflating the abdomen with gas (pneumoperitoneum), which can put pressure on the heart. However, with modern anesthesia monitoring and our in-house cardiologist Dr. Manjunath D, we safely perform these procedures on patients with cardiac history after thorough optimization.
Answer: The synthetic mesh is permanent. It is designed to integrate with your tissues and stay there for life. It does not degrade or need replacement unless it gets infected (which is very rare).
Answer: Laparoscopy leaves 3 tiny scars (0.5 to 1 cm) which fade significantly over time. They are often barely noticeable compared to the 10cm scar of open surgery.
Answer: The risk of recurrence with laparoscopic mesh repair is very low (<1-2%). However, factors like smoking, obesity, and straining can increase this risk. This is why our functional medicine team works with you to manage these lifestyle factors.
A hernia is more than a bulge; it is a breach in the fortress of your body. Ignoring it invites risk, but treating it requires precision. At ARKA Anugraha Hospital, we blend the technical mastery of a Center of Excellence with the compassionate, holistic care of a family practice.
From the molecular understanding of your connective tissue to the ergonomic travel plans for our Mysore patients, every detail of your journey is curated for success. We invite you to leave the pain and uncertainty behind and trust your care to the experts who are defining the standards of hernia surgery in South India.
Take Action Today:
ARKA Anugraha Hospital
#2, 15th Cross Rd, 6th Phase, J. P. Nagar, Bengaluru, Karnataka 560078
Phone: +91-8073737505
Your Health, Our Excellence.
BEST Institute was started with the intention of sharing my knowledge with
other fellow surgeons. During this journey, many conferences and workshops
have been conducted. Skills training is the highlight of this Institute.
December 3, 2025 What is Hernia and How Can It Be Treated with Laparoscopy? Executive Summary: The Structural Integrity of the…
November 19, 2025 What is Bariatric Surgery and Who Should Consider It? What is Bariatric Surgery and Who Should Consider It?…
October 2, 2024 NATIONAL CONFERENCE & WORKSHOP ON HERNIA Blog Dates: 27th& 28th March 1999 Venue: St. Martha’s Hospital, Bangalore This…